There are around 100,000 – 200,000 ACL injuries in the USA each year which lead to altered biomechanics, increased risk of re-injury and development of osteoarthritis.
EMG can provide feedback on asymmetries and rate of force development which is critical for sporting tasks involving jumping or cutting maneuvers.
EMG decomposition techniques have shown alterations in motor unit recruitment patterns that can provide vital information for return to play strategies and rehabilitation.
POP! The sound that any athlete will dread hearing. The popping sound has become synonymous with a rupture of the anterior cruciate ligament (ACL). Commonly injured in dynamic sporting activities during pivoting, cutting, or jumping maneuvers, the ACL has plagued the careers of many top professional athletes, but also hampered daily activities of recreationally active individuals. In the US alone, there are between 100,000 and 200,000 ACL injuries with individuals then being predisposed to a 6 times greater risk of re-injury and an 87% chance of developing osteoarthritis within 15 years. These contributing factors have led to the injury becoming one of the most studied within biomechanics.

"The level of detail provided by EMG decomposition is pivotal for understanding the mechanisms behind persistent muscle weakness and for developing more targeted rehabilitation strategies.”
Dr. Dave Sherman, Northeastern University
ACL Injuries in the US per Year
Greater Risk of Re-injury
Chance of Developing Osteoarthritis
The ACL is not only an important stabilizing ligament of the knee, but also provides essential feedback on joint position and loading, which are key to motor planning and control. Rehabilitation is therefore pivotal for an individual’s successful return to sport and overall well-being. But what are the best ways to assess rehabilitation outcomes? This blog explores some of the latest science and technologies that are pushing the field forward within ACL rehabilitation.
ACL injuries result in biomechanical and neuromuscular alterations and quadriceps dysfunction is almost ubiquitous across ACL reconstruction patients. Persistent quadricep weakness and atrophy are key struggles that result in altered movement mechanics and these movement deficits can often be seen through vision inspection and kinematic analysis. However, it has been seen that there are high levels of symmetry for maximal torque producing capacity between the injured and uninjured limbs at the time of return-to-play. This prompts the question as to why movement mechanics are still altered if maximal strength capacity is not noticeably diminished. To answer this, Dr. Daniel Cobain, as seen in the seminar presentation, suggests that perhaps we need to focus on functional assessments that replicate the demands of the sporting task.
Most ACL injuries happen during dynamic sporting activities. During these tasks, characterized by alternating periods of activation and relaxation lasting roughly between 100ms and 300ms, the requirement for performance is not often solely about how much force you can produce, but instead about how quickly you can produce the force. The measure of rapid muscle activation is frequently described as the rate of force development (RFD). Dr. Cobain describes that when assessing the RFD within ACL reconstruction patients, this is when we see a large change as patients struggle to activate the injured limb’s quadriceps at the same rate as the uninjured limb.
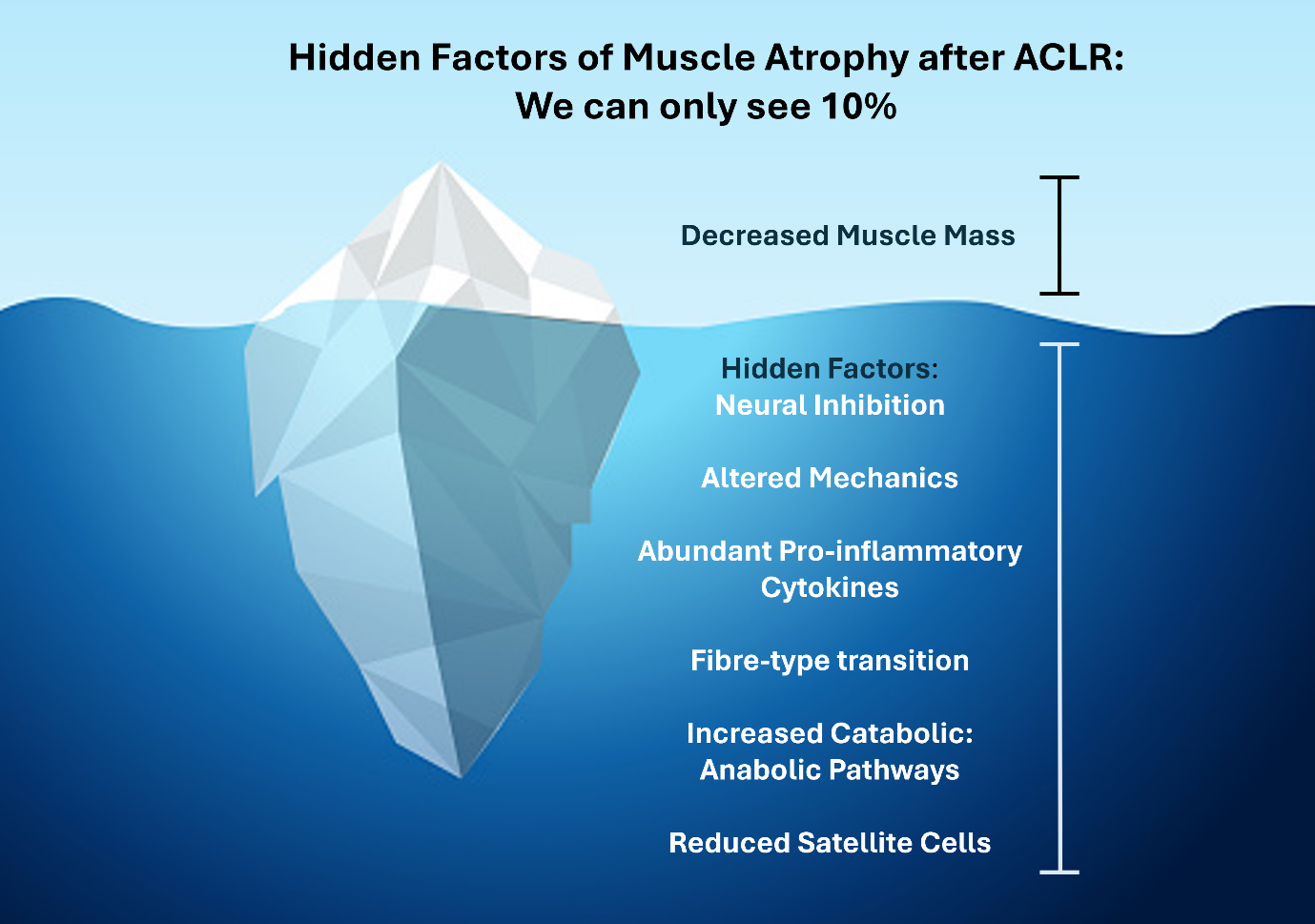
While surface EMG can provide strong feedback to inform return to play rehabilitation protocols, to fully understand where the underlying neuromuscular deficits lie, we perhaps need to dive into the single motor unit level data via EMG decomposition techniques. Recent research has come to light for how motor unit data can enable a deeper understanding of neuromuscular impairments post-ACL injury, which is crucial for addressing the root cause of muscle weakness effectively.
Motor units are the collective term for the motoneuron and the groups of muscle fibres it innervates. Muscle activation, and hence force production, is encoded by the total number of activated motor units and the rate at which the motoneurons discharge action potentials.
We spoke to Dr. Dave Sherman, an incoming assistant professor at Northeastern University, about some of his recent research into ACL rehabilitation and motor unit modulations:
Our research questions focus on how ACL injuries and rehabilitation affect the neural control of the quadriceps. We aim to trace the origin of clinical impairments to pinpoint modifiable treatment targets. This involves exploring the relationship between motor unit behavior and neural activity at spinal and cortical levels to assess how neural drive modulation impacts motor unit behavior.”
By using the Delsys NeuroMap system and Trigno Galileo sensors, the group have been able to uncover notable results.
We’ve found that at the time of return to unrestricted activity, the quadriceps’ motor unit recruitment patterns are altered, favoring the early recruitment of larger, slower motor units. This finding, not fully explained by spinal cord excitability or muscle activation failure, indicates that suboptimal motor unit behavior might develop early in rehabilitation and persist beyond clinical recovery. Emerging evidence points to possible cortical involvement in later recovery stages through diminished neural drive to the quadriceps, a discovery made possible by the detailed analysis enabled by decomposition EMG.”
Dr. Sherman added that the level of insight would only be possible through decomposition techniques.
These new technologies enable a deeper understanding of neuromuscular impairments post-ACL injury, offering insights into the relationships between motor unit size, firing rates, and recruitment thresholds, crucial for addressing muscle weakness effectively.”
One of the biggest questions that still remains is how we can take research findings and apply these to clinical and practical settings in rehabilitation. In the ISEK around the world event, Macarena Soldan presented a view from working with EMG and motor unit decomposition to help inform clinical steps.
Dr. Sherman furthered these points and stated that, within their own work, the next steps will be looking to advance the clinical adoption of new interventions:
There’s substantial evidence supporting interventions like focal joint cooling, neuromuscular electrical stimulation, and biofeedback for treating muscle inhibition. Understanding their impact on motor unit behavior will pave the way for creating neurofeedback interventions that address the root causes of impairments. This progression is crucial for enabling clinicians to assess these impairments in clinical settings and to apply effective interventions to tackle them directly.”
To take meaningful steps forward in the treatment of ACL injuries and mitigate against long-lasting side effects, a deeper understanding of neural drive and muscle inhibition via advanced sensing technologies will only promote more effective treatment plans for healthier and better rehabilitated patients.
To learn more about how EMG technologies can support your work, reach out to contact@delsys.com.




